In the spring of 2020, as the pandemic created a worldwide shortage of N95 masks, two Stanford engineers working out of their homes designed and demonstrated an effective yet inexpensive way to disinfect personal protective equipment (PPE).
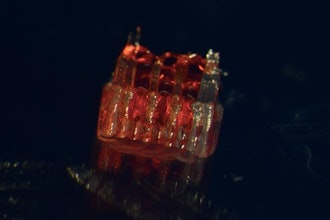
In two papers recently published in the journal Applied Optics, they described how they used ultraviolet light (UV) to deactivate a bacterium that is accepted as a proxy for the dangerous-to-handle virus that causes COVID-19.
"We were surprised when testing indicated that our process could eliminate 99.9999 percent of pathogens in under five minutes," says Thomas Baer, executive director of the Stanford Photonics Research Center (SPRC) and senior author of the two publications, one on building the units and the other on the basic engineering principles.
Baer's principal collaborator on the project was Lambertus "Bert" Hesselink, a professor of electrical engineering and optics expert, who helped to provide the proofs that light-based decontamination would be feasible and effective. They each designed a prototype mask sterilization device to serve as a model for do-it-yourself photonics engineers around the world to copy for use wherever they might be.
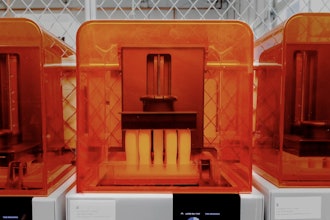
Baer built the first prototype by lining a storage cabinet with aluminum foil and installing 16 UV light fixtures to create a device that could sterilize 40 masks in just five minutes. He likens it to a large toaster oven. "Toast needs to be toasted evenly and the masks need to be exposed evenly," Baer explains. "It's the same geometry with a very similar design goal."
Hesselink developed an alternative design that took advantage of the shape of a metal garbage can to uniformly expose masks to pathogen-killing UV rays. Based on Hesselink's design, Baer built this smaller device in about three hours, then went on to demonstrate that this small sterilizer could be run on solar power. "The can design decontaminates fewer masks at a time, but it is easily transported, requires minimal power and can be used in remote areas," Hesselink said.
After submitting their scientific papers for peer review, Baer and his collaborators worked closely with a Stanford-organized international group of scientists (N95Decon.org), helping public health teams in limited-resource settings use inexpensive, locally sourced components to build their own decontamination units. "These are simple, do it yourself, open-source models, designed specifically to be easily constructed in these settings," Baer says.
To provide these foreign sites with local engineering know-how, the Stanford team collaborated with two organizations with a global reach -- Lifebox, a London-based nonprofit with a medical focus, and the Optical Society Foundation, which has an international network of photonics engineers. With these groups, the Stanford team helped launch 25 do-it-yourself efforts around the world to build UV-based decontamination units for local hospitals.
One such effort is being led by Jit Bhattacharya, who earned his master's degree in mechanical engineering from Stanford in 2002 and now lives in Nairobi, Kenya. He had been working to develop energy technologies, but when the pandemic broke out, he started looking for ways join the fight against COVID-19, found the Stanford design and realized it could be assembled locally. Bhattacharya now plans to demonstrate a prototype to the Kenyan Ministry of Health and at several Kenyan hospitals. He says that given what hospitals in Kenya are currently paying for N95 masks, the UV cabinet would pay for itself in weeks by enabling health care workers to safely reuse their N95 masks rather than disposing of them.
On the domestic front, Baer and Hesselink are working with researchers at the Wellman Center for Photomedicine at Massachusetts General Hospital to secure U.S. Food & Drug Administration approval for UV decontamination chambers based on their design. "Many people were designing ultraviolet sterilization chambers without a clear understanding of the necessary design constraints," Baer says. "Our publications demonstrated the appropriate optical engineering tools and performance goal, as well as some very simple construction examples."