Bleeding is the most common cause of potentially survivable death in trauma, in both military and civilian settings. Whole blood is recognized as the resuscitation fluid of choice; however, it has limited viability, requires cold storage, and is not always available due to logistical challenges and donor dependence. Despite the Department of Defense’s (DoD) extensive and highly effective blood program, rapid patient evacuation to a facility that has blood is not always an option. To improve changes for survival, patients should have access to blood in 30 minutes or less.
DARPA’s Fieldable Solutions for Hemorrhage with bio-Artificial Resuscitation Products (FSHARP) program aims to develop a field-deployable, shelf-stable whole blood equivalent that can be used to resuscitate trauma patients when donated blood products are not available.
“When blood donations decline – as we have seen during the COVID pandemic – that threatens availability everywhere, even in high resource settings. Blood availability also could be at risk in military engagements with large numbers of casualties, with a sudden and significant increase in need,” stated Cmdr. Jean-Paul Chretien, DARPA’s program manager for FSHARP and a U.S. Navy medical officer. “The primary problem FSHARP aims to solve is whole blood’s dependence on cold chain and resupply.”
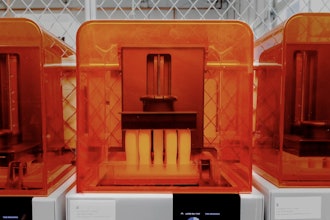
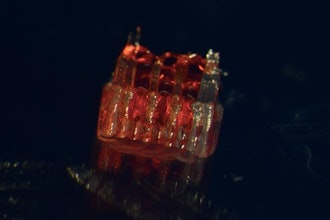
DARPA selected a team at the University of Maryland, Baltimore (UMB) to lead this effort with support from Case Western Reserve University, Charles River Laboratories, Haima Therapeutics, KaloCyte Inc., Latham Biopharm Group, Ohio State University, Pumas-AI Inc., Southwest Research Institute, Teleflex Incorporated, University of California San Diego, and University of Pittsburgh. Their plan is to integrate multiple bio-artificial and synthetic components to deliver oxygen, stop bleeding, and replace volume—key therapeutic functions of whole blood in resuscitation. They will evaluate efficacy and safety in increasingly complex and realistic trauma models, and intend to develop strategies for stabilizing the product for months without cold storage and scalable manufacturing methods.
Other subcontractors have the potential to join the UMB consortium pending the exercise of additional options in the FSHARP award.
“This is truly a ‘DARPA Hard’ problem and an example of DARPA’s ability to facilitate the partnerships needed to achieve technological breakthroughs,” added Chretien. “To address FSHARP’s goals requires multiple universities and companies developing analogues of various blood components, simultaneous evaluation of multiple efficacy and safety features and interactions among components in various model systems, industrial-scale manufacturing capabilities that can adapt the lab-scale methods, and analytics to integrate large volumes of experimental data and guide further optimization. UMB has assembled a consortium with the broad set of capabilities needed to accomplish these tasks.”