Scientists from UNSW Sydney have developed a ceramic-based ink that may allow surgeons in the future to 3D-print bone parts complete with living cells that could be used to repair damaged bone tissue.
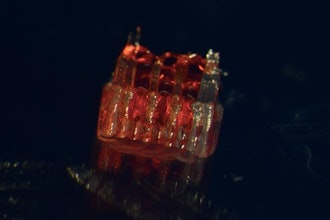
Using a 3D-printer that deploys a special ink made up of calcium phosphate, the scientists developed a new technique, known as ceramic omnidirectional bioprinting in cell-suspensions (COBICS), enabling them to print bone-like structures that harden in a matter of minutes when placed in water.
While the idea of 3D-printing bone-mimicking structures is not new, this is the first time such material can be created at room temperature - complete with living cells - and without harsh chemicals or radiation, says Dr. Iman Roohani from UNSW's School of Chemistry.
"This is a unique technology that can produce structures that closely mimic bone tissue," he says.
"It could be used in clinical applications where there is a large demand for in situ repair of bone defects such as those caused by trauma, cancer, or where a big chunk of tissue is resected."
Associate Professor Kristopher Kilian who co-developed the breakthrough technology with Dr. Roohani says the fact that living cells can be part of the 3D-printed structure, together with its portability, make it a big advance on current state-of-the-art technology.
Up until now, he says, making a piece of bone-like material to repair bone tissue of a patient involves first going into a laboratory to fabricate the structures using high-temperature furnaces and toxic chemicals.
"This produces a dry material that is then brought into a clinical setting or in a laboratory, where they wash it profusely and then add living cells to it," Professor Kilian says.
"The cool thing about our technique is you can just extrude it directly into a place where there are cells, like a cavity in a patient's bone. We can go directly into the bone where there are cells, blood vessels and fat, and print a bone-like structure that already contains living cells, right in that area."
"There are currently no technologies that can do that directly."
In a research paper published recently in Advanced Functional Materials, the authors describe how they developed the special ink in a microgel matrix with living cells.
"The ink takes advantage of a setting mechanism through the local nanocrystallisation of its components in aqueous environments, converting the inorganic ink to mechanically interlocked bone apatite nanocrystals," Dr. Roohani says.
"In other words, it forms a structure that is chemically similar to bone-building blocks. The ink is formulated in such a way that the conversion is quick, non-toxic in a biological environment and it only initiates when ink is exposed to the body fluids, providing an ample working time for the end-user, for example, surgeons."
He says when the ink is combined with a collagenous substance containing living cells, it enables in-situ fabrication of bone-like tissues which may be suitable for bone tissue engineering applications, disease modeling, drug screening, and in-situ reconstruction of bone and osteochondral defects.
Already there has been keen interest from surgeons and medical technology manufacturers. Prof. Kilian thinks while it's early days, this new bone-printing process could open up a whole new way of treating and repairing bone tissue.
"This advance really paves the way for numerous opportunities that we believe could prove transformational - from using the ink to create bone in the lab for disease modeling, as a bioactive material for dental restoration, to direct bone reconstruction in a patient," says Prof. Kilian.
"I imagine a day where a patient needing a bone graft can walk into a clinic where the anatomical structure of their bone is imaged, translated to a 3D printer, and directly printed into the cavity with their own cells.
"This has the potential to radically change current practice, reducing patient suffering and ultimately saving lives."
Next up the duo will be performing in vivo tests in animal models to see if the living cells in the bone-like constructs continue to grow after being implanted in existing bone tissue.